Understanding the FDA’s Final CDS Guidance
The Final Clinical Decision Support (CDS) Guidance, describes the FDA’s regulatory approach to Clinical Decision Support (CDS) software functions. Suffice it to say that much of the previously designated non-device CDS software might no longer be considered as a non-medical device based on the final CDS guidance.
We developed a comprehensive comparison of Final and Draft CDS Guidance to allow you to understand the key differences. Rook Quality Systems has extensive experience helping clients (i.e., CDS software manufacturers) draft and file premarket submissions, pre-submissions, and 513(g) applications. Please do not hesitate to contact us if you have any questions.
Overview of the CDS Guidelines
FDA initially issued a draft guidance interpreting these criteria in 2017, and given stakeholder feedback, issued a revised draft guidance in 2019. The Final CDS Guidance was issued in September 2022:
- The Final CDS Guidance streamlines the Draft CDS Guidance by focusing the scope on CDS intended to be used by state licensed, registered, or certified health care professionals, rather than those also used by patients and caregivers, which were included in the scope of the Draft CDS Guidance.
- The Draft CDS Guidance’s detailed discussion and application of the IMDRF final document entitled “Software as a Medical Device: Possible Framework for Risk Categorization and Corresponding Considerations” is absent from the Final Guidance.
- The Final Guidance also contains clearer organization and examples to identify FDA’s views on non-device CDS software functions and device software functions.
Final CDS Guidance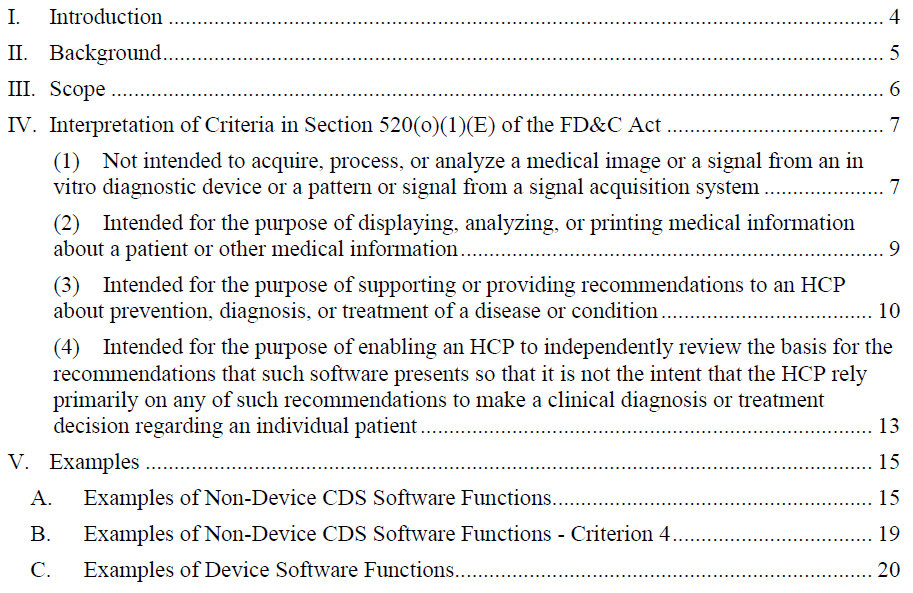
2019 CDS Guidance Draft
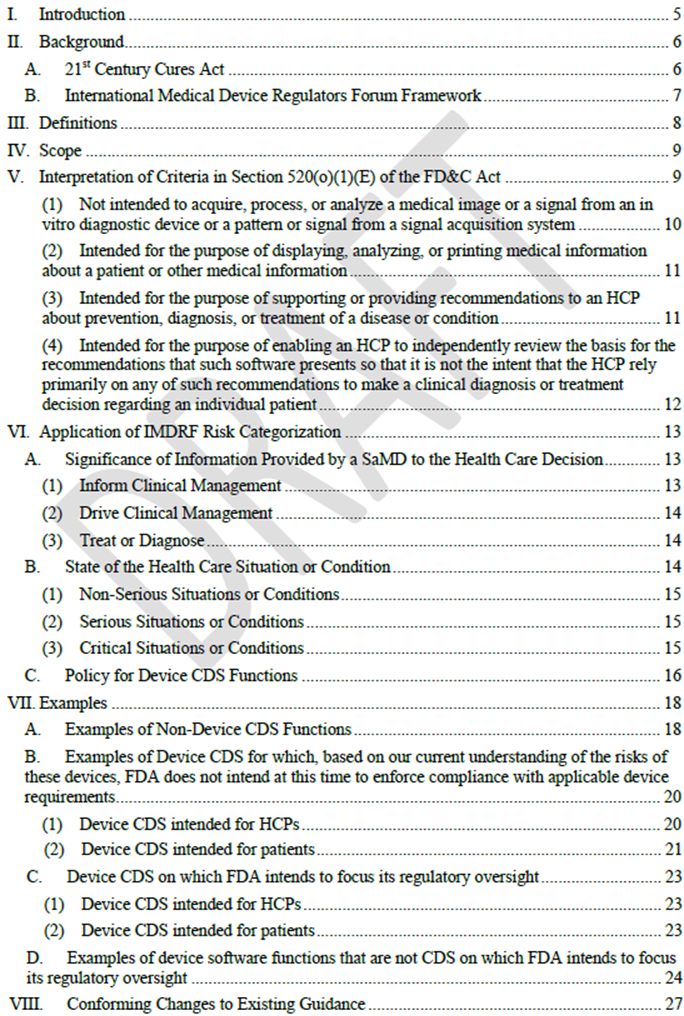
Difference between 2019 and Final version of CDS guidance
1. Device Exclusion Criteria
Criterion 1:
The CDS Final Guidance is largely consistent with its approach in the 2019 draft guidance.
- The addition of a definition of the term “pattern” (defined as multiple, sequential, or repeated measurements of a signal or from a signal acquisition system) and inclusion of some additional examples.
- “Medical image” to include any image analyzed for a medical purpose including images not originally taken for a medical purpose.
- Datasets such as variant call format (VCF) files constitute patterns from a signal acquisition system, suggesting that CDS functions that analyzes VCFs would not meet Criterion 1.
Criterion 2:
The CDS Final Guidance includes significant changes to FDA’s interpretation of this criterion. FDA’s narrow interpretation of medical information in Criterion 2 would exclude potentially relevant information that is not yet well understood and accepted.
- “medical information about a patient” refers to the type of information typically communicated between HCPs in a clinical conversation or between HCPs and patients in the context of a clinical decision
- “other medical information” to include information such as peer-reviewed clinical studies, clinical practice guidelines, and information that is independently verified and validated as accurate, reliable, not omitting material information, and supported by evidence
Criterion 3:
FDA eliminated the IMDRF framework from its 2019 CDS draft guidance and the key principle that software could be classified on the basis of whether it “drives” or “informs” clinical management.
- FDA’s prior 2017 and 2019 draft guidance documents provided little discussion of Criterion 3, and most stakeholders had generally taken a broad interpretation of software outputs that could be a CDS recommendation.
- The exclusion of CDS that provides a specific output or that supports time-critical decision-making is new and could narrow the scope of CDS. Software that provides “a specific preventative, diagnostic, or treatment output or directive”—including software that provides information that a patient may exhibit signs of a disease or identifies a risk probability or risk score for a disease—does not meet Criterion 3.
Criterion 4:
In response to comments on the 2019 draft guidance raising questions about the type of information needed to satisfy the transparency requirement in Criterion 4, the CDS Final Guidance includes several tangible recommendations on satisfying this criterion.
- Usability testing may be necessary to determine whether implementation of CDS software meets the fourth criterion
2. Additional Examples of Device and Non-Device CDS
Additionally, FDA provides over 30 examples of device software functions for which FDA intends to exercise regulatory oversight, many of which are new additions from the draft guidance.
Narrowed Focus on Software Intended for HCPs
The CDS Final Guidance streamlines the 2019 draft guidance by eliminating the discussion of patient/caregiver-directed CDS that existed in the previous guidance. These patient/caregiver-directed tools are also referred to as patient decision support (“PDS”).
- PDS must be analyzed under FDA’s other digital health policies, including FDA’sPolicy for Device Software Functions and Mobile Medical Applications; Software as a Medical Device (SaMD): Clinical Evaluation; Medical Device Data Systems, Medical Image Storage Devices, and Medical Image Communication Devices; and General Wellness: Policy for Low Risk Devices.
- The 2019 draft guidance proposed that FDA exercise enforcement discretion for certain CDS intended for use by patients or caregivers and certain CDS for use by HCPs intended to inform management of a non-serious situation or condition. The Final CDS Guidance does not discuss a policy of enforcement discretion for either category. Instead, FDA merely states that some decision support software may be subject to enforcement discretion under the Agency’s other digital health guidances.
4. FDA has not addressed how it will apply the Final CDS Guidance
The Final CDS Guidance provides no discussion of how industry should apply the many changes in the guidance or how the Agency will view software on the market under the prior guidance documents that now may not meet the criteria for Non-Device CDS under the revised interpretations in the Final CDS Guidance. For example, FDA included no discussion of an effective compliance date for the new interpretation in the Final CDS Guidance or a transition period to allow industry to make corresponding changes.
Perspective and Recommendations on the Changes
Based on our extensive experience working with CDS software, we anticipate that there will be many software functions on the market or in development that no longer fall within Non-Device CDS under FDA’s Final CDS Guidance or under enforcement discretion under FDA’s other digital health guidance. It is imperative that CDS software manufacturers- particularly those who develop CDS software intended for caregivers and patients and CDS software which provides a specific output or directive- carefully reassess their software function under the criteria per the Final CDS Guidance, and determine the impact of changes on the regulatory strategies. FDA has not specified any transition or compliance period, so manufacturers will want to act quickly to assess these impacts, develop a strategy, and potentially engage with FDA regarding impacted software. Look to Rook for more insights and guidance on this trending topic.
